Abstract
Background
Sickle cell disease (SCD) is one of the most common and devastating inherited blood disorders characterized by a single nucleotide mutation in the beta-globin chain leading to the production of mutant hemoglobin S (HbS). HbS polymerizes upon deoxygenation causing red blood cells (RBC) to sickle which results in extremely painful episodes of vaso-occlusive crisis (VOC), severe hemolytic anemia, chronic multiorgan failure and a reduced life span. An important metabolic feature directly associated with RBC sickling is increased intracellular levels of the glycolytic intermediate 2,3-diphosphyglycerate (2,3-DPG) which promotes deoxygenation by lowering the oxygen affinity of hemoglobin (Hb). Pyruvate kinase R (PKR) is a key enzyme in RBC metabolism, generating adenosine triphosphate (ATP) to maintain energy homeostasis, membrane integrity and deformability, and modulates 2,3-DPG levels. Mitapivat (AG-348) is an oral, small molecule allosteric activator of PKR and shows promise as an anti-sickling agent in addition to its effect in PK deficiency and thalassemia. The safety and efficacy of mitapivat in subjects with SCD was evaluated in the dose finding period of this ongoing phase 2 study.
Methods
The ESTIMATE study is a phase 2, open-label study in which subjects ≥16 years with SCD (HbSS, HbS/β0, HbS/β+) with a baseline hemoglobin >6.1 g/dL and ≤11.1 g/dL, no chronic transfusion and adequate organ function were eligible. In the 8-week Dose Finding Period, initial dosing of mitapivat was 20 mg twice daily (BID). Subjects received a maximum of two sequential dose escalations of mitapivat (i.e. from 20 mg BID to 50 mg BID and 100 mg BID) depending on safety. The primary endpoints were safety, evaluated by frequency and severity of adverse events (AEs), and efficacy of mitapivat on RBC sickling. RBC sickling was evaluated by change in Point of Sickling (PoS), the pO2 at which sickling occurs as measured by oxygen gradient ektacytrometry on the Lorrca (RR Mechatronics). Secondary endpoints included changes in hematological parameters, levels of 2,3-DPG and ATP, Hb-oxygen affinity (p50) and surrogate markers of organ damage and mortality. Subjects who safely tolerated mitapivat and showed evidence of clinical improvement, were eligible to continue a 52-week follow-up period (Fixed Dose Extension Period).
Results
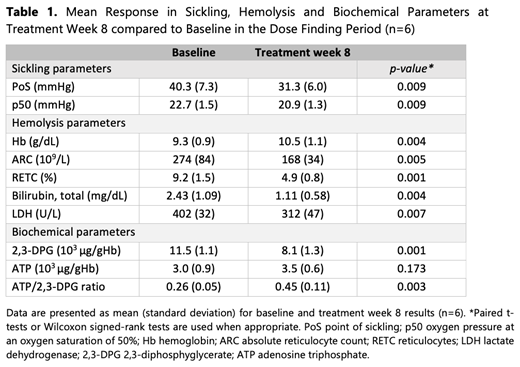
Six subjects have been enrolled as of September 2020 and completed the Dose Finding Period. All had homozygous HbSS except one patient who had HbS/β0-thalassemia. Baseline characteristics were: median age of 36 years (range 20-59 years), 4 (66.7%) were female and 5 (83.3%) were on stable-dose hydroxyurea. All subjects received dose escalation to a maximum dose of 100 mg BID. No serious adverse events (SAEs) occurred. Adverse events (AEs) were mild and often transient, with the most common treatment emergent AEs: transaminase increase (n=3 [50.0%], Grade 1), gastrointestinal disorders including dyspepsia, diarrhea and abdominal discomfort (n=3 [50.0%], Grade 1) and headache (n=2 [33.3%], Grade 1). One VOC occurred without hospital admission and did not require dose reduction or discontinuation. Table 1 summarizes the anti-sickling effect as well as the hematological and biochemical response to mitapivat treatment. Sickling occurred at lower pO2 levels in all 6 patients during the Dose Finding Period reflected by a significant decrease in treatment week 8 mean PoS compared to baseline. 5/6 subjects (83.3%) achieved a Hb increase of ≥1 g/dL during this period, which was accompanied by a decrease in hemolytic markers. Consistent with activation of PKR, 2,3-DPG levels decreased and ATP levels increased. Additional results including biomarker data will be presented.
Conclusion
Mitapivat demonstrated an adequate safety profile during the 8-week Dose Finding Period in patients with SCD. The data show promising efficacy in terms of a decrease in the pO2 at which RBCs start to sickle, as well as increase in Hb from baseline and a concomitant decrease in markers reflecting hemolysis. The observed changes in 2,3-DPG and ATP levels are consistent with the proposed mechanism of the drug. The study is ongoing and further data including follow-up data, patient-reported outcomes, PKR activity and thermostability will be reported at a later stage.
van Dijk: Agios Pharmaceuticals: Research Funding; Axcella Health: Research Funding. Rab: Axcella Health: Research Funding; Agios Pharmaceuticals: Research Funding. Rijneveld: Servier: Research Funding; Amgen: Research Funding. Nur: Celgene: Speakers Bureau; Novartis: Research Funding, Speakers Bureau; Roche: Speakers Bureau. Schutgens: CSL Behring: Research Funding; Novo Nordisk: Research Funding; OctaPharma: Research Funding; Pfizer: Research Funding; Shire/Takeda: Research Funding; Bayer: Research Funding. Wijk: Agios Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Research Funding; Axcella health: Research Funding; Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding. Van Beers: Pfizer: Research Funding; Novartis: Research Funding; Agios Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Research Funding; RR Mechatronics: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal